Hand Care Issues
Intact skin is a first line defence mechanism against infection. Damaged skin can not only lead to infection in the host, but can also harbour higher numbers of microorganisms than intact skin and hence increase the risk of transmission to others. Damaged skin on healthcare workers is an important issue and needs to be seriously addressed.
Click here for an example of a skin care questionnaire for healthcare workers.
There are two major types of skin reactions associated with hand hygiene. Irritant contact dermatitis; which includes symptoms that can vary from mild to debilitating, including dryness, irritation, itching, and even cracking and bleeding. The other being allergic contact dermatitis, which is rare and represents an allergy to some ingredient in a hand hygiene product. In its most serious form allergic contact dermatitis may be associated with symptoms of anaphylaxis.
The vast majority of skin problems among healthcare workers that are related to hand hygiene are due to “irritant contact dermatitis”. Irritant contact dermatitis is primarily due to frequent and repeated use of hand hygiene products - especially soaps, other detergents, and paper towel use, which result in skin drying. The initial use of alcohol-based handrubs among such healthcare workers often results in a stinging sensation. However, recent studies have suggested that the ongoing use of emollient-containing alcohol-based handrub leads to improvement in irritant contact dermatitis in approximately 70% of affected healthcare workers. Also, the use of an oil-containing lotion or a barrier cream three times a shift can substantially protect the hands of vulnerable healthcare workers against drying and chemical irritation, preventing skin breakdown.
It is important to ensure that the selected alcohol-based handrub, soaps, and moisturising lotions are chemically compatible to minimise skin reactions among staff.
Factors that may contribute to dermatitis include:
- Fragrances and preservatives. Commonly the cause of contact allergies; these should be kept to a minimum or eliminated when selecting an ABHR
- Washing hands regularly with soap and water immediately before or after using an alcohol-based handrub is not only unnecessary, but may lead to dermatitis
- Donning gloves while hands are still wet from either handwashing or applying alcohol-based handrub increase the risk of skin irritation
- Using hot water for handwashing
- Failure to use supplementary moisturisers
- Quality of paper towels
The management of hand care problems associated with the use of hand hygiene products requires early recognition and a systematic approach to ensure success.
Strategies for minimising occupational hand dermatitis include:
- Use of a hand hygiene product that contains skin emollient to minimise the risk of skin irritation and drying
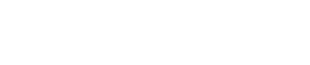
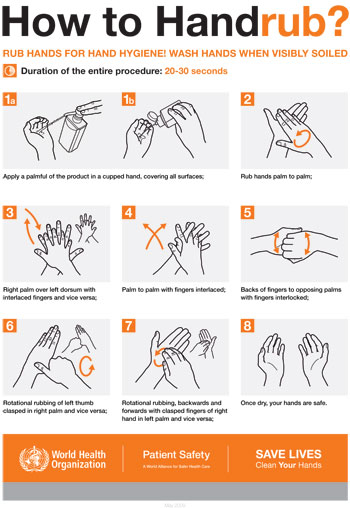
- Educating staff on the correct use of hand hygiene products
- Educating staff on caring for their hands, including the regular use of skin moisturisers both at work and at home - such moisturising skin-care products need to be compatible with alcohol-based handrubs
- Providing a supportive attitude towards staff with skin problems
Alcohol-based handrub produces the lowest incidence of irritant contact dermatitis of all the hand hygiene products currently available. True allergy to alcohol-based handrub is rare and allergy to alcohol alone has not been reported.
Although some reports have suggested that irritant contact dermatitis can occur in up to 30% healthcare workers; the incidence of this problem among a recent study of Victorian healthcare workers was extremely low (0.47%), representing one cutaneous adverse event per 72 years of healthcare worker exposure.
Healthcare workers should be encouraged to notify the hand hygiene lead if skin irritation occurs following the use of alcohol-based handrub. All complaints should be taken seriously and a review process instigated. All hospitals should have access to referral for follow up that may include: an Occupational Dermatologist, local Doctor, or emergency department for healthcare workers with persistent skin problems. For WHO consensus recommendations on skin care see Appendix 6 in the HHA Manual.
Cutaneous Absorption
Recent studies have demonstrated minimal rates of cutaneous alcohol absorption such that there should be no concern for healthcare workers. A study suggested that isopropanol might be less likely to be absorbed than ethanol. Thus, healthcare workers concerned about absorption for religious reasons may elect to use an alcohol-based handrub that contains isopropanol rather than ethanol.
Cultural and religious factors strongly influence attitudes to community handwashing which, according to behavioural theorists are likely to have an impact on compliance with hand hygiene during health care. In some religions, and even within the same religion, various degrees of interpretation exist concerning alcohol prohibition. In general, those religions with an alcohol prohibition in everyday life demonstrate a practical view accepting the most valuable approach to optimal patient care. Consequently, no objection is raised against the use of alcohol based products for environmental cleaning, disinfection or hand hygiene.
When implementing a hand hygiene campaign with an alcohol-based handrub in a healthcare setting where religious groups are represented, it is important to include focus groups on this topic to allow healthcare workers to raise concerns about the use of alcohol-based handrubs, help them to understand the evidence underlying this recommendation, and to identify possible solutions to overcome obstacles. The same process should be used when implementing alcohol-based handrubs into areas where there may be a cultural problem with alcohol abuse.
Further Information And Resources
- - Flow chart for management from the Occupational Dermatology Education and Research Centre
- The website of the Occupational Dermatology Education and Research Centre